When Sleep Struggles Look Like ADHD: What Parents Should Know
Sleep struggles can affect focus, behavior, and emotional regulation. This article explores how poor sleep can sometimes look like ADHD - and why addressing sleep first can bring clarity.
Many parents start asking questions about focus, behavior, or emotional regulation only after months (or years) of poor sleep.
They might say things like:
“My child can’t focus.”
“Their emotions feel so big.”
“Everything feels harder when they’re tired.”
Sometimes, those concerns raise questions about ADHD. Other times, parents simply know something feels off but can’t quite name it.
What’s often missed in these conversations is how closely sleep and nervous system regulation are connected, and how sleep struggles can sometimes look like ADHD, especially in young children.
Sleep and regulation are deeply connected
Sleep isn’t just rest for the body. It’s a regulatory process for the nervous system.
When a child sleeps well, their nervous system has more capacity to:
Focus
Manage emotions
Adapt to stress
Transition between activities
When sleep is fragmented or difficult, that same nervous system may stay in a more reactive state during the day.
Why poor sleep can affect focus and behavior
A tired nervous system has fewer resources.
When sleep isn’t restorative, parents may notice:
Short attention span
Increased impulsivity
Emotional outbursts
Difficulty transitioning
Sensory sensitivity
Big reactions to small stressors
These behaviors can resemble ADHD traits, especially when viewed without the full context of sleep quality and regulation.
This doesn’t mean sleep “causes” ADHD.
It means sleep can amplify regulation challenges.
When sleep struggles come first
In many families, sleep challenges appear long before concerns about focus or behavior.
Parents often describe:
Difficulty settling at bedtime
A child who seems constantly overtired
More intense behavior on poor-sleep days
This pattern matters because a nervous system that never fully rests may struggle to regulate during the day.
This doesn’t mean ADHD is “just sleep.”
This is an important distinction.
ADHD is a neurodevelopmental diagnosis. It is not caused by sleep problems, and sleep support is not a replacement for appropriate evaluation or care.
However, sleep quality plays a foundational role in how symptoms are expressed, perceived, and managed.
For some children:
Supporting sleep improves regulation
Focus becomes easier
Emotional responses soften
For others:
Sleep support becomes an important piece of a bigger picture
Both can be true.
Why addressing sleep first often brings clarity
When sleep improves, parents and providers gain clearer information.
Better sleep can help answer questions like:
Are behaviors still present when the child is well-rested?
Does focus improve when regulation improves?
Are challenges consistent across environments?
This clarity can be incredibly helpful for families navigating next steps.
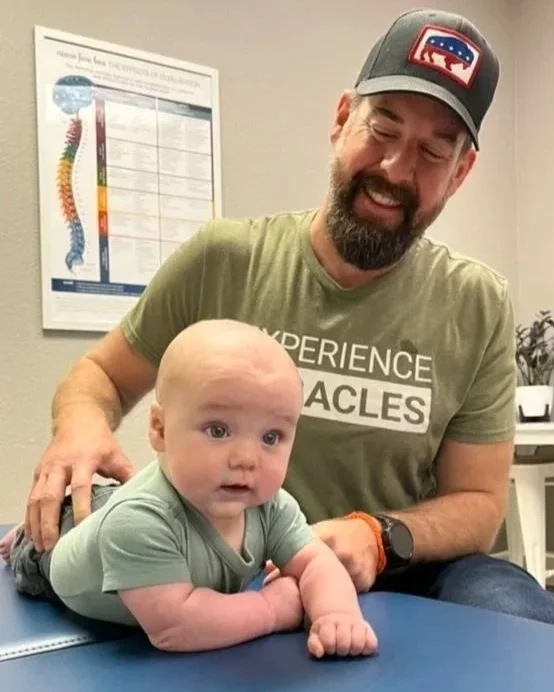
How Pediatric Chiropractic Center views sleep and regulation
At Pediatric Chiropractic Center, we look at sleep, behavior, and focus through a nervous system lens.
Our role is not to diagnose ADHD or replace medical care.
Our role is to help identify and support patterns of nervous system stress that may be impacting regulation, both day and night.
Sleep is often one of the first places those patterns show up.
When to consider deeper support
You may want to explore additional support if:
Sleep challenges have been ongoing
Daytime regulation feels increasingly difficult
Your child seems constantly overtired
Behavior worsens after poor sleep
Your intuition says something more is going on
Parents are often the first to notice when sleep and regulation are connected.
A calm next step for parents
If you’re wondering whether sleep, regulation, and focus may be connected for your child, you’re not alone - and you don’t need all the answers right now.
Understanding sleep is often the first step toward understanding regulation more broadly. Next steps: Learn more about sleep and nervous system regulation. For families navigating an ADHD diagnosis or ongoing focus concerns, understanding the broader role of the nervous system can provide helpful context.
Dr. Matt McCormack, DC, CCSP, CPPFC
Sleep Training vs Nervous System Regulation: What Parents Should Know
Sleep training doesn’t work for every child. This article explains how nervous system regulation differs from behavior-based sleep strategies and why readiness matters.
Few parenting topics feel as loaded as sleep training.
Many parents come into our office asking:
“Do I have to sleep train?”
“Is sleep training bad for my baby?”
“Why didn’t sleep training work for us?”
These are valid questions - and the answer is often more nuanced than what’s found online.
This article explains the difference between sleep training and nervous system regulation, and why understanding that difference matters.
In a hurry? Here’s the short answer
Sleep training focuses on behavior.
Nervous system regulation focuses on physiology.
For some children, sleep strategies work easily.
For others, sleep struggles persist because the body isn’t fully ready to relax - no matter how consistent the routine.
What sleep training is designed to do
Sleep training methods generally aim to:
Teach independent settling
Reduce night wakings
Create predictable sleep patterns
These approaches assume that a child’s nervous system is:
Capable of self-soothing
Able to shift into rest
Comfortable transitioning between sleep cycles
For some children, this is true.
For others, it’s not - yet.
Why sleep training doesn’t work for every child
When sleep training fails, parents are often told:
“Be more consistent”
“They’re testing boundaries”
“You just need to stick with it longer”
But if a child’s nervous system is under stress, consistency alone doesn’t solve the problem.
Signs sleep training may not align with a child’s needs include:
Escalating distress
More frequent night wakings
Short naps
Increased daytime dysregulation
A child who sleeps better when supported than when alone
What nervous system regulation focuses on instead
Nervous system regulation looks at why sleep is difficult, not just how to change it.
This includes considering:
How easily a child shifts into a calm state
Whether the body can fully relax
Sensory sensitivity
Digestive comfort
Tension patterns
Stress from birth or illness
When regulation improves, sleep often becomes:
Easier to initiate
Deeper
Less fragmented
More sustainable
Sleep training vs regulation: not always either/or
This is important to say clearly:
Sleep training and nervous system regulation are not enemies.
Some families:
Choose sleep training
Modify sleep strategies
Or wait until regulation improves before introducing changes
What matters most is whether the child’s nervous system is ready.
Why some babies only sleep with support
One common reason parents feel conflicted about sleep training is contact sleep.
Babies who:
Wake immediately when placed down
Need constant support
may not yet have the physiological capacity to self-settle.
How PCC approaches sleep conversations
At Pediatric Chiropractic Center, we don’t push a single sleep philosophy.
We focus on:
Supporting regulation
Helping parents make informed choices
The goal is not to force independence - it’s to help sleep feel safer and easier over time.
When to pause, modify, or rethink sleep strategies
You may want to reconsider your approach if:
Sleep strategies increase distress
Your child becomes more overtired
Daytime behavior worsens
Your intuition says something isn’t right
Parents are not failing when sleep strategies don’t work - they may simply be responding to a child who needs more regulation first.
Final thoughts for parents
You don’t have to choose sides.
Understanding your child’s nervous system gives you context, clarity, and confidence - whether you sleep train, modify strategies, or wait.
Sleep isn’t about willpower.
It’s about readiness.
Dr. Matt McCormack, DC, CCSP, CPPFC
Baby Won’t Sleep Unless Held? What This Can Mean for Your Child’s Nervous System
If your baby will only sleep when held and wakes the moment you put them down, you’re not doing anything wrong. Learn what contact sleep can signal about nervous system regulation and how to gently support more restful sleep.
If your baby will only sleep when held - and wakes the moment you put them down - you’re not creating bad habits.
You’re responding to your baby’s need for comfort and regulation.
For many families, this pattern isn’t about sleep training or routines. It’s about how a baby’s nervous system is responding to stress, comfort, and safety.
This guide explains why contact sleep happens, what it can signal, and how to gently support your baby toward more restful sleep.
In a hurry? Here’s the short answer
When a baby only sleeps when held, it often means:
Their nervous system settles best with external regulation (aka co-regulation)
They have difficulty fully relaxing on their own
Sleep transitions feel unsafe or uncomfortable
Contact provides pressure, warmth, and safety cues
This is common, biological, and not a parenting failure.
Why contact sleep is so common (especially in babies)
Newborns and young infants are not born with mature self-regulation.
They rely on:
Touch
Movement
Warmth
Heartbeat
Breath rhythm
Holding provides all of these at once.
When a baby is placed down, especially if their nervous system is already under stress, the sudden loss of these cues can trigger a startle or waking response.
This isn’t manipulation - it’s survival physiology.
What contact sleep can tell us about regulation?
Many babies outgrow contact sleep naturally as their nervous systems mature.
However, when contact sleep persists despite consistent routines, it may indicate:
Heightened startle reflex
Sensory sensitivity
Digestive discomfort
Tension patterns in the body
Stress from birth, illness, or developmental transitions
Signs your baby may need more support beyond routines
Parents often notice:
Waking every 30–60 minutes
Needing to be held all night
Short naps that only happen on a parent
Strong startle when placed down
Better sleep during motion than stillness
Fussiness or stiffness during transitions
These signs don’t mean something is “wrong” - they suggest the nervous system may need additional support.
Why “just put them down drowsy” doesn’t always work
Advice like:
“Put them down awake”
“They need to learn”
“You’re creating habits”
assumes the nervous system is ready to self-settle.
For some babies, it isn’t - yet.
Trying to force independence before regulation is in place often leads to:
More waking
More distress
More exhaustion for everyone
Sleep improves when the body feels safe enough to let go.
What can help support your baby’s nervous system?
Gentle regulation support may include:
Predictable rhythms (not rigid schedules)
Reducing daily sensory overload
Supporting digestion and comfort
Gentle movement and pressure
Addressing tension patterns
Consistent, calm bedtime cues
These strategies work best when paired with an understanding of why your baby seeks contact in the first place.
How Pediatric Chiropractic Center approaches contact sleep
At Pediatric Chiropractic Center, we view contact sleep through a nervous system lens.
Our approach focuses on:
Identifying stress patterns
Supporting regulation
Helping the body transition into rest more easily
The goal is not to eliminate contact prematurely - it’s to help sleep become more comfortable and sustainable over time.
When to consider additional support
You may want to seek further evaluation if:
Sleep has not improved over time
Your baby seems chronically overtired
Daytime regulation is difficult
Feeding or reflux concerns are present
Your intuition says something deeper is happening
Parents are often the first to recognize when sleep struggles go beyond routine tweaks.
Take the next step
If your baby won’t sleep unless held and you feel stuck, you’re not alone - and support is available!
Learn more about sleep and nervous system regulation
Dr. Matt McCormack, DC, CCSP, CPPFC